Social prescribing involves a trusted referrer connecting a person to a link worker, who acts as a resource while the individual creates their own personalised plan, identifying opportunities and avenues for enrichment to enhance their quality of life.
Social prescribing involves a trusted referrer connecting a person to a link worker, who acts as a resource while the individual creates their own personalised plan, identifying opportunities and avenues for enrichment to enhance their quality of life.
Social prescribing – What is it?
Social prescribing – the evidence base
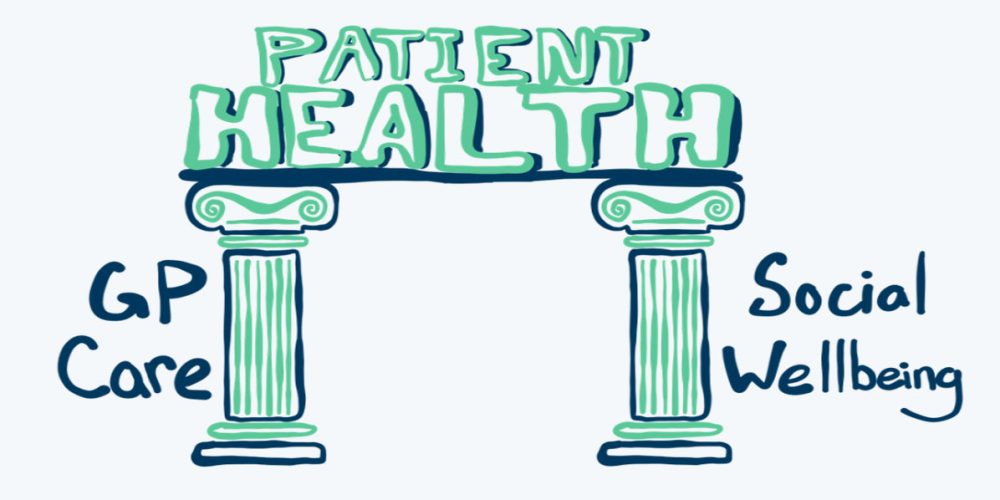
Social prescribing is a growing framework used by GPs and other health practitioners internationally, particularly in the UK. It shares the same values as the broader person-centred care approach that now underpins the health and social care sectors.
 Based on evidence from overseas social prescribing initiatives where pilot programs have been successful, a first of its kind program was launched in Australia in 2017: Plus Social® for injured workers. Now, Plus Social is also available on the Gold Coast and is tailored to support people whose lives are significantly impacted by mental ill-health. It is funded by the Gold Coast Primary Health Network and will link patients with non-medical sources of support within the community. The program aims to address the social and health gaps those with severe mental illness may experience.
Based on evidence from overseas social prescribing initiatives where pilot programs have been successful, a first of its kind program was launched in Australia in 2017: Plus Social® for injured workers. Now, Plus Social is also available on the Gold Coast and is tailored to support people whose lives are significantly impacted by mental ill-health. It is funded by the Gold Coast Primary Health Network and will link patients with non-medical sources of support within the community. The program aims to address the social and health gaps those with severe mental illness may experience.
in South Eastern NSW, PCCS offers Social Rx®, another social precribing program to help people tackle the non-medical barriers to their health and wellbeing, including issues such as housing, social and community networks, family relationships and other socioeconomic factors that a person and their doctor cannot address alone. We work with people to identify meaningful goals and to develop a personalised plan to meet these needs while reducing isolation and disadvantage.
The following is a summary of four key pieces of evidence which support the use of social prescribing and an additional selection of eight other relevant references. The majority of currently available evidence comes out of the UK.
Review of 86 social prescribing schemes in the UK, 2015
 This review looked at 86 UK social prescribing schemes and found that just over 40% of these programs had been formally evaluated. The review found evidence that social prescribing delivers the following benefits for participants and that these are especially pronounced for marginalised groups: enhanced self-esteem and confidence, a greater sense of control and empowerment, improved mental wellbeing and mood, reduced social isolation and loneliness, improved motivation and the acquisition of new skills. It also found social prescribing reduces the number of visits to primary and secondary care services, including GPs.
This review looked at 86 UK social prescribing schemes and found that just over 40% of these programs had been formally evaluated. The review found evidence that social prescribing delivers the following benefits for participants and that these are especially pronounced for marginalised groups: enhanced self-esteem and confidence, a greater sense of control and empowerment, improved mental wellbeing and mood, reduced social isolation and loneliness, improved motivation and the acquisition of new skills. It also found social prescribing reduces the number of visits to primary and secondary care services, including GPs.
Thomson, L.J., Camic, P.M. & Chatterjee, H.J. (2015). Social Prescribing: A review of community referral schemes. London: University College London https://repository.canterbury.ac.uk/download/b4200c5d0d0b31dfd441b8efedffae2865b13569e44cb4a662898a3ed20c1092/3729872/Social_Prescribing_Review_2015.pdf
Review of seven linking schemes in the UK, 2015
 The review considered seven UK studies in which referrals were usually made through general practices. Almost all interventions involved a facilitator who identified and linked participants to suitable community-based services. The review found evidence to support improvements to participant’s psychosocial wellbeing and reduced usage of health services. It also found “the involvement of health professionals in aiding the referral of patients to the intervention and the role of the intervention facilitators as key components of the interventions.” (p467)
The review considered seven UK studies in which referrals were usually made through general practices. Almost all interventions involved a facilitator who identified and linked participants to suitable community-based services. The review found evidence to support improvements to participant’s psychosocial wellbeing and reduced usage of health services. It also found “the involvement of health professionals in aiding the referral of patients to the intervention and the role of the intervention facilitators as key components of the interventions.” (p467)
Mossabir R, et al. A scoping review to understand the effectiveness of linking schemes from healthcare providers to community resources to improve the health and well-being of people with long-term conditions. Health & Social Care in the Community 2015;23(5) 467-484, https://onlinelibrary.wiley.com/doi/abs/10.1111/hsc.12176
Evaluation of a social prescribing service in Rotherham (UK), 2016
 This is an evaluation of the Social Prescribing Service in Rotherham (UK) that is delivered by Voluntary Action Rotherham in partnership with over 20 local community and voluntary organisations. The service is one of the largest in the UK and has continued to operate since commencing as a two year pilot in 2012.
This is an evaluation of the Social Prescribing Service in Rotherham (UK) that is delivered by Voluntary Action Rotherham in partnership with over 20 local community and voluntary organisations. The service is one of the largest in the UK and has continued to operate since commencing as a two year pilot in 2012.
The service model involves GPs referring eligible patients and carers to a team of link workers who provide access to voluntary and community support for patients and GPs as well as funding these voluntary and community organisations to provide additional activities suited to participants. It aims to help GPs to better meet the non-clinical needs of patients with complex long-term conditions. During the three year evaluation period, more than 2,000 people had substantively engaged with the service. The evaluation found that participants had reduced demand for urgent hospital care (including a 17% reduction in emergency department attendances), improved wellbeing, reduced social isolation and better self-management of their condition.
Dayson, C., Bashir, N., Bennet, E. & Sanderson, E. (2016). The Rotherham Social Prescribing Service for People with Long-Term Health Conditions: Annual Evaluation Report. Rotherham/Sheffield: Voluntary Action Rotherham (VAR) and Centre for Regional Economic and Social Research (CRESR). https://www.artshealthresources.org.uk/docs/evaluation-of-the-rotherham-mental-health-social-prescribing-service-2015-16-2016-17/
Evaluation of a linking service in Wigan (UK), 2016
 This report evaluates the Wigan Community Link Worker service that was established to improve health and wellbeing through enabling better connections to appropriate supports within the community. It commenced as a pilot and involved 63 practices. Health professionals working in primary care, hospitals and social care could refer people to link workers who identified participant’s needs and aspirations and then facilitated their access to appropriate community supports and activities. The evaluation considered 784 participants and largely uses qualitative data. It found the service has had “significant impact on the lives of its clients, for example, helping people in crisis to tackle and resolve issues quickly and supporting people with longer term challenges to build confidence, develop plans and make behaviour changes through becoming active in the community.” (p36). The greatest impact was derived from the time the link workers spent actually listening to the participants. Other impacts on participants included: access to improved relationships of participants with families and friends, greater involvement in the community and enhanced social networks, improved confidence and greater motivation. Benefits to GPs were found to include freeing up of GP time thereby allowing more effective use of primary care resources and enabling the role of GPs to be expanded to connect people with community resources.
This report evaluates the Wigan Community Link Worker service that was established to improve health and wellbeing through enabling better connections to appropriate supports within the community. It commenced as a pilot and involved 63 practices. Health professionals working in primary care, hospitals and social care could refer people to link workers who identified participant’s needs and aspirations and then facilitated their access to appropriate community supports and activities. The evaluation considered 784 participants and largely uses qualitative data. It found the service has had “significant impact on the lives of its clients, for example, helping people in crisis to tackle and resolve issues quickly and supporting people with longer term challenges to build confidence, develop plans and make behaviour changes through becoming active in the community.” (p36). The greatest impact was derived from the time the link workers spent actually listening to the participants. Other impacts on participants included: access to improved relationships of participants with families and friends, greater involvement in the community and enhanced social networks, improved confidence and greater motivation. Benefits to GPs were found to include freeing up of GP time thereby allowing more effective use of primary care resources and enabling the role of GPs to be expanded to connect people with community resources.
Innovation Unit (May 2016). Wigan Community Link Worker Service Evaluation. https://www.innovationunit.org/wp-content/uploads/2017/05/Wigan-CLW-service-evaluation.pdf
Additional references
- Kilgarriff-Foster, A., O’Cathain, A. Exploring the components and impact of social prescribing. Journal of Public Mental Health 2015; 14(3) 127-134. https://core.ac.uk/reader/42620510
- Chatterjee, H.J., Camic, P.M., Lockyer, B., Thomson, L.J.M. Non-clinical community interventions: a systematised review of social prescribing schemes. Arts & Health; 2017. https://www.tandfonline.com/doi/full/10.1080/17533015.2017.1334002
- Laing, K. et al. (2017) How Ways to Wellness social prescribing is improving the health and wellbeing of people with long term conditions: Evaluation report to the Cabinet Office. University of Newcastle (UK); Institute of Health & Society. https://golab.bsg.ox.ac.uk/documents/105/Laing_et_al._2017a.pdf
- Moffatt, S. et al. Link Worker social prescribing to improve health and well-being for people with long-term conditions: qualitative study of service user perceptions. British Medical Journal Open 2017; 7:e015203. http://bmjopen.bmj.com/content/bmjopen/7/7/e015203.full.pdf
- Kimberlee, R. (2013) Developing a social prescribing approach for Bristol. Project Report. Bristol Health & Wellbeing Board, UK. http://eprints.uwe.ac.uk/23221/1/Social%20Prescribing%20Report-final.pdf
- Bragg, R., Wood, C. & Barton, J. (2013). Ecominds effects on mental wellbeing: An evaluation for Mind (University of Essex). Stratford/London: Mind. https://www.mind.org.uk/media-a/4418/ecominds-effects-on-mental-wellbeing-evaluation-report.pdf
- Langford, K., Baeck, P. & Hampson, M. (2013) More than medicine: New services for people powered health. London: Nesta2 https://www.nesta.org.uk/documents/151/more_than_medicine.pdf
Learn more
 The latest research is also being collected and furthered by the recently established Australian Social Prescribing Institute of Research and Education (ASPIRE).
The latest research is also being collected and furthered by the recently established Australian Social Prescribing Institute of Research and Education (ASPIRE).
Find out more about the institute at their website, CreatingOpportunitiesTogether.com.
Partner with us!
Social Rx is an innovative program designed and delivered by PCCS throughout parts of NSW and the Gold Coast (QLD). If your organisation is interested in adding Social Rx to the service options available for your region, send us a message on our contact form or email us here to discuss and learn more.